Brain Surgery and Neurosurgical Oncology
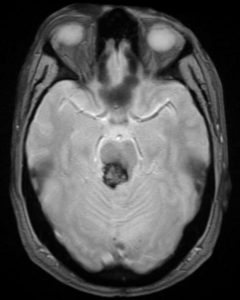
Cavernoma (Cavernous angioma)
On this page, Dr Christian Brogna explains what a brain cavernoma is, who it affects, presenting symptoms and the choice of the best treatment.
What is a cavernoma or cavernous angioma?
A cavernoma is a roundish, blackberry-like formation made up of abnormal vessels.
It can be present in the brain, cerebellum, brainstem, or spinal cord.
Cavernous angioma, cavernous hemangioma, and cavernous brain malformation (CCM cavernous brain malformations) are all synonymous with cavernoma.
How big are the cavernomas? Are they tumors?
Cavernomas can measure from a few millimeters to a few centimeters. The stagnation of blood in their structure can cause them to increase in size.
However they are not brain tumors and as such they do not metastasize to other parts of the body.
Can cavernomas bleed?
Sometimes the cells that form the vessels that make up the cavernoma can rupture and leak blood into the cavernoma or out directly into the brain or spinal cord.
It is very difficult to accurately predict when a cavernoma will bleed and to quantify the neurological damage it will cause.
How common are cavernomas?
About 1 in 600 people have a brain cavernoma.
This means that about 95,000 people in Italy harbour a brain cavernoma (as many as the Olympic Stadium in Rome contains.
About 1 in every 400,000 people are diagnosed with a brain cevernoma each year.
Spinal cord cavernomas are rarer than cerebral cavernomas.
How many cavernomas have a genetic basis?
Almost 50% of cavernomas are thought to be linked to a genetic condition. The rest is made up of sporadic forms.
They can also appear after radiation therapy.
20% of patients have multiple cavernomas and many of these have a positive family history.
When to perform a genetic counseling?
Patients with multiple cavernomas or symptomatic patients with family members with genetically based cavernomas should be tested.
If the patient is not symptomatic, he/she can perform the genetic test, but must be clear about the psychological impact in case it is found to be positive (a genetic counseling before administering the test is paramount).
The genes involved and tested are CCM1 (KRIT1), CCM2 (MGC4607), and CCM3 (PDCD10).
The disease is inherited with an autosomal dominant character.
Patients with a CCM3 gene mutation are quite young and have a higher risk of having cutaneous cavernomas, scoliosis, spinal cavernomas, neurocognitive disabilities, meningiomas, gliomas, neuromas.
How do brain cavernomas manifest? What symptoms?
Cavernomas can cause symptoms for three reasons:
- hypersensitization of the brain circuits around the cavernoma (epilepsy) (50%).
Repeated microhemorrhages on the onset of epileptic seizures; - Increase in size of the cavernoma with compression of brain structures and neurological deficits (25%);
- Bleeding (25%).
The risk of hemorrhage from a cavernoma is estimated to be around 15% in 5 years, and decreases over time.
Patients in whom the cavernoma is localized in the brainstem and present with haemorrhage for the first time have a higher risk of re-bleeding.
The most common symptoms are:
- epileptic crisis;
- headache;
- paresis of one or more limbs or part of the face;
- speech disorder, tremors, double vision, balance disorder;
- sensitivity disturbance, memory, concentration disturbance.
Some cavernomas can be diagnosed when a CT scan or MRI is done for other reasons (such as a head injury).
These are defined as “incidental” (25-50%).
How are cavernomas diagnosed?
Cavernomas are diagnosed with CT scan (in an emergency) and with MRI.
The neurosurgeon may request some specific magnetic resonance sequences that are used to understand the relationship between the cavernoma and the brain structures responsible for specific functions (for example, speech functions or motor functions).
How are cavernomas treated? What is their treatment of choice?
The decision on the most suitable treatment for each individual patient should only be made after careful neurosurgical evaluation.
In fact, there are many factors that play a role in the final decision (age, location of the cavernoma, symptoms, whether single or multiple, whether there is a genetic condition or not, etc.).
After surgery, patients who have experienced seizures are more likely to permanently resolve these seizures.
In those cases manifesting with epileptic seizures it is advisable to operate as soon as possible, since after one year the seizures may become more refractory to therapies even after surgery.
The treatment of choice, when indicated, is surgical resection of the cavernoma.
Bibliography:
Synopsis of Guidelines for the Clinical Management of Cerebral Cavernous Malformations: Consensus Recommendations Based on Systematic Literature Review by the Angioma Alliance Scientific Advisory Board Clinical Experts Panel.
Neurosurgery. 2017 May 1;80(5):665-680. doi: 10.1093/neuros/nyx091.
Akers A1, Al-Shahi Salman R2, A Awad I3, Dahlem K1, Flemming K4, Hart B5, Kim H6, Jusue-Torres I7, Kondziolka D8, Lee C1, Morrison L9, Rigamonti D7, Rebeiz T3, Tournier-Lasserve E10, Waggoner D11, Whitehead K12.
